The cost of healthcare in the United States has always been a hot-button issue, but every so often, a story emerges that leaves people questioning the boundaries of reason. One such story recently went viral, involving a young woman who was charged for something so seemingly ordinary that it shocked thousands online. This unexpected fee wasn’t for a test, a procedure, or even a consultation—it was for an emotional response. As the details unfolded, it became clear that this wasn’t just an isolated case but a window into the broader complexities and frustrations of navigating the American healthcare system.
The $40 Charge: What Happened?
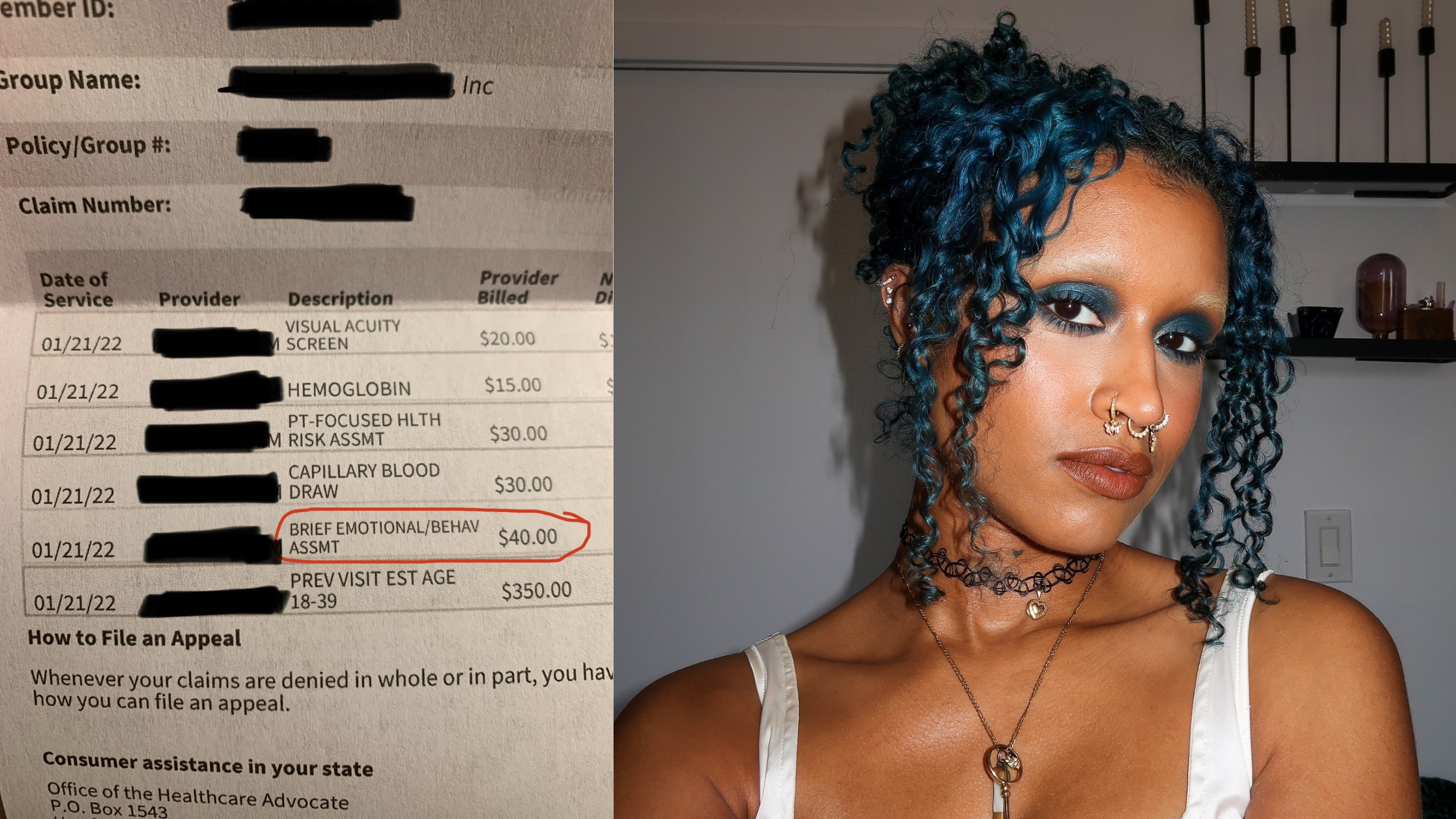
In early 2022, Camille Johnson, a 25-year-old content creator from Brooklyn, New York, shared a startling experience involving her younger sister’s medical visit. Her sister, who had been grappling with a rare health condition, finally secured a doctor’s appointment. Overwhelmed by the situation, she shed a tear during the consultation. Later, when reviewing the itemized medical bill, they discovered a $40 charge labeled as a “brief emotional/behavioral assessment.” Camille expressed her frustration on Twitter, stating, “One tear in and they charged her $40 without addressing why she is crying, trying to help, doing any evaluation, any prescription, nothing.”
This incident is not isolated. A 2020 study published in JAMA found that 1 in 5 insured adults in the U.S. received an unexpected medical bill from an out-of-network provider in the past two years.
The public reaction to Camille’s tweet was swift and widespread, with many sharing similar experiences of unexpected medical charges. One user recounted being billed $1,902 for a pregnancy test labeled as “Women’s services,” while another mentioned a $44 fee for “skin to skin contact” after childbirth.
Understanding Emotional/Behavioral Assessments

The $40 charge labeled as a “brief emotional/behavioral assessment” on Camille Johnson’s sister’s medical bill corresponds to CPT code 96127. This code is defined as a brief emotional or behavioral assessment using standardized instruments, including scoring and documentation. It’s commonly used for screenings related to depression, anxiety, attention-deficit/hyperactivity disorder (ADHD), and substance abuse.
The implementation of CPT code 96127 aligns with the Affordable Care Act (ACA), which mandates that mental health services be included as essential benefits in all insurance plans. This initiative aims to ensure that mental health screenings are a routine part of medical care, promoting early detection and intervention for mental health conditions.
However, in the case of Johnson’s sister, the application of this code appears to have been misused. According to Johnson, her sister was not evaluated for any mental health conditions during the visit. She stated, “They did not evaluate her for depression or other mental illnesses, nor did they discuss her mental health with her.” This discrepancy highlights a potential issue where the code may be applied without the corresponding service being provided, leading to unexpected charges for patients.
A study published in the Journal of Behavioral Health Services & Research emphasizes that while the ACA has expanded coverage for mental health services, the consistent and appropriate application of these services remains a challenge. Ensuring that patients receive the assessments they’re billed for is crucial for maintaining trust in the healthcare system.
The Broader Issue: Healthcare Transparency
A significant factor contributing to this opacity is the use of chargemasters—comprehensive lists of billable services and their prices maintained by healthcare providers. These lists are typically not disclosed to patients, leading to confusion and mistrust when unexpected charges appear on medical bills. As noted in a New Yorker article, the complexity and secrecy surrounding chargemasters have been criticized for contributing to the high costs of healthcare.
The lack of transparency in medical billing has tangible consequences. A study published in the Journal of Medical Internet Research found that despite mandates for hospitals to publish pricing information, the data is often presented in formats that are not user-friendly, hindering patients’ ability to make informed decisions about their care.
The implications of opaque billing practices are profound. Patients may delay or forgo necessary medical care due to fear of unforeseen costs, potentially leading to worsened health outcomes. Moreover, unexpected medical bills can contribute to financial strain, with medical debt being a leading cause of bankruptcy in the United States.
Addressing these challenges requires systemic changes to promote transparency and rebuild trust between patients and healthcare providers. Implementing clear, accessible billing practices and ensuring patients are informed about potential costs upfront are essential steps toward a more equitable healthcare system.
The Public Reaction and Online Debate
The public reaction to Camille Johnson’s revelation about her sister being charged $40 for crying during a doctor’s appointment was swift and widespread. Many individuals shared their own experiences with unexpected medical charges, highlighting systemic issues within the U.S. healthcare system.
One Twitter user recounted, “I got charged over $2,000 for an emergency room trip for a nosebleed that wouldn’t stop. I had to wait so long, the nurse moved me into a room because I was bleeding all over the waiting room. Doc never saw me; it stopped bleeding before he arrived.”
Another individual shared, “My daughter was charged $44 for ‘skin-to-skin contact.’ In other words, when they flopped my grandson up onto her chest after the umbilical cord was cut. I guess the cheaper alternative was letting him fall on the floor?”
These personal accounts resonated with many, prompting discussions about the transparency and ethics of medical billing practices. The collective outrage underscored a growing demand for systemic reforms to address the financial burdens imposed on patients.
In response to the widespread attention, Camille Johnson emphasized the need for change, stating, “We need a drastic change in the healthcare industry, and I thought that sharing a real-life story online would be a good way to open up the conversation and help advocate for change.”
The online debate highlighted a pervasive sentiment: that the commodification of basic human experiences within the healthcare system is both ethically questionable and indicative of deeper systemic issues. As one commenter aptly put it, “Tell me you live in America without telling me that you live in America.”
Tips for Navigating Medical Bills
Navigating medical bills can be daunting, especially when unexpected charges arise. Here are some practical steps to help manage and potentially dispute such bills:
- Request an Itemized Bill: Always ask for a detailed breakdown of charges. This allows you to identify any discrepancies or unexpected fees, such as the $40 charge for a “brief emotional/behavioral assessment” in Camille Johnson’s sister’s case.
- Review Bills for Errors: Billing errors are not uncommon. Common mistakes include double billing, upcoding, or charges for services not rendered. A study in JAMA Health Forum highlights that self-advocacy in identifying and correcting these errors can lead to financial relief.
- Understand Your Insurance Coverage: Familiarize yourself with your insurance policy to know what services are covered and to what extent. This knowledge can help you spot charges that should have been covered by your insurer.
- Communicate with Healthcare Providers: If you identify an unexpected charge, contact the billing department of the healthcare provider. A respectful and clear inquiry can often resolve misunderstandings or errors. As noted by Patient Fairness, preparing and sending a letter of dispute promptly can obligate the provider to address your concerns.
- Negotiate Bills: Don’t hesitate to negotiate medical bills. Many providers offer discounts for prompt payment or can set up interest-free payment plans to ease financial strain.
- Seek Financial Assistance: Hospitals and clinics often have financial assistance programs for patients facing financial hardships. Inquire about eligibility to reduce your medical expenses.
- Document All Communications: Keep detailed records of all interactions with healthcare providers and insurance companies, including dates, names of representatives, and summaries of discussions. This documentation can be crucial if disputes escalate.
- Consult a Patient Advocate: If the process becomes overwhelming, consider seeking help from a patient advocate. They can assist in understanding bills, disputing charges, and negotiating with providers. Patient advocates can improve health outcomes and prevent errors by facilitating communication between patients and healthcare providers.
- Be Aware of Legal Protections: Familiarize yourself with laws designed to protect patients from unfair billing practices, such as the No Surprises Act, which aims to prevent unexpected medical bills.
- Stay Informed and Proactive: Regularly review medical statements and Explanation of Benefits (EOBs) from your insurer. Prompt attention to discrepancies can prevent minor issues from becoming significant financial burdens.
A Call for Compassion in Healthcare
The story of Camille Johnson’s sister being charged $40 for crying during a medical visit has become a symbol of the broader issues plaguing the American healthcare system. From a lack of transparency in billing practices to unexpected fees that exacerbate financial and emotional burdens, the challenges patients face are undeniable.
At its core, healthcare should prioritize empathy and patient well-being. The commodification of basic human experiences, such as an emotional response, highlights the urgent need for systemic reforms. Greater transparency, clear communication, and ethical billing practices are essential steps toward restoring trust and dignity in healthcare.
As public outrage over stories like these grows, it’s clear that change is possible, but it requires collective action. Patients, advocates, and policymakers must work together to ensure that the healthcare system reflects its ultimate purpose: to heal, support, and care for those in need, without undue financial strain or unnecessary distress. This story serves as a reminder that every voice counts in the fight for a more compassionate and transparent system.